Acoustic Noise in MRI
-Parajuli
K, MSc Medical Imaging, IOM, Nepal
Why
noise is a problem in MRI1
·
It causes discomfort, anxiety and
distraction to the patient.
·
It causes problem in verbal communication.
·
It can cause discomfort in sedated
patients.
·
Some medications can increase the
sensitivity of our ear to sound.
·
Temporary shift in the threshold of
hearing has been reported.
·
Neonates have increased sensitivity to
acoustic noise.
·
Unwanted activation of auditory cortex
during functional MRI causes spurious patterns and is a serious problem.2
How
is noise produced in MRI
There are many sources
of noise in mri.
They can be categorized
into four groups
a. Due to gradient
current
b. Due to eddy current
c. Due to radio
frequency waves and slice selection pulse
d. Due to ambient noise
Noise
due to gradient current3
Gradient,
spatial variation in magnetic field is produced by the electric currents
flowing through coil. Large pulsed electrical current ranging from 200 A to
600A with rise time in the order of sub millisecond or millisecond is applied
to copper windings held together by epoxy resin and fiber glass. Gradient coil is
itself situated in the magnet bore assembly and thus experience the main
magnetic field, a force called Lorentz force develops in between the gradient
current and static magnetic field, which causes bending and buckling the coil
producing compressional force. Force of 2000 N per meter of gradient coil is
produced resulting in vibrations with acceleration levels in the order of 100 m/s2. Lorentz
force is given by the relation:
where dl is the
element inside the magnetic field.
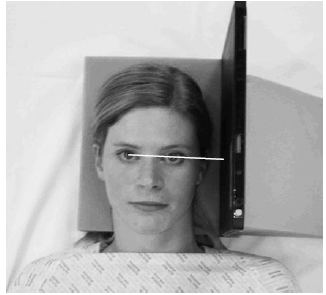
Fig
1: grey arrow showing the direction of gradient current and white arrow shows
direction of Lorentz force.
Figure (2) shows
two mode of vibration: cone shaped vibration in Z gradient (A) and banana
shaped vibration in X-Y gradient (B).
Studies have
shown similarity between spectrum of gradient current and that of noise. Also,
amplitude of vibration is higher when frequency of gradient current matches the
resonant frequency of gradient coil which depends on properties of length and
elastic properties of material in coil assembly. It is thought to be due to better
acoustic transfer function of the gradient system at resonant frequency. The
time course of the gradient current depends on various pulse sequence
parameters (TR, TE, FOV). Thus pulse sequence can be modified such that
frequency of gradient current (also the frequency of vibration) does not match
the resonant frequency of the coil. In EPI the frequency of readout gradient
can be adjusted such that it is not same as resonant frequency of the gradient
coil.
In addition, the
wave for gradient can be changed from trapezoidal to sinusoidal.
Noise
due to eddy current4
Gradient magnetic field
induces eddy current, according to faradays law of electromagnetic induction,
in the metallic structures located in the vicinity of the gradient coil for eg.
inner cryostat in superconducting systems and Rf body coil, Rf shield etc.
These structures conducting the eddy current are situated in a magnetic field
because of which Lorenz force develops and induces vibration. Recent study by
Eldestein et al 4have shown that main source of noise in MRI is due
to eddy current induced vibration of the conducting structures located near the
gradient coil.
RF
Hearing1
It is due to pressure
waves generated because of expansion of tissues as a result of rise in
temperature (1x10-6 degrees C) caused by the RF induced heating. It
is very nominal compared to gradient field induced acoustic noise and there is
no proof regarding harmful effects due to RF hearing.
Ambient
noise3
Inside the scanner room
there are various other sources of noise for example:
1.
Noise due to air blower of air handling
system that can produce noise upto 20 dbA.
2.
Pounding sound of low frequency due to
liquid helium pump that can reach up to 80 dB.
How
much is the noise produced in MRI5, 6
Noise level in MRI depends
upon the hardware construction and surrounding environment i.e the presence and
absence of various structures that reflect sound. Thus sound level is measured
in specific pressure level or sound pressure level which can be expressed in
linear or A-weighted scale. The sensitivity of human ear depends upon the frequency
of sound. A-weighted sound takes into account the different sensitivity of
human ear to various frequencies of sound and is expressed as dBA or dB(A).dB(A)
is better correlated with the risk of noise induced hearing loss.
Noise levels of 70 to
130 dB have been reported. Price et al found noise level to be 82.5+-0.1 dB (A)
in 0.23 to 0.5T systems and 118.4 +-1.3 dB (A) in 3T systems. Hattori et al6
found that noise in 3T MR systems exceeded that of regulatory limit of 99 dB
given by IEC. The peak sound pressure level was 125.7 dB for MR angiography,
130.7dB for SS-EPI (single shot spin echo EPI) on the linear scale.
What
factor affects level of noise produced?
It depends upon the
scan parameters like section thickness, FOV, TR and TE. It is because change in
these parameters bring about change in gradient output (rise time and
amplitude).Smaller the section thickness and FOV and shorter the TR, higher is
the level of noise produced. It increases logarithmically with increase in
magnetic field.
Studies have shown
presence and absence of patient can also create difference in level of acoustic
noise produced. The value was found to be larger in the former case.
What
are the regulatory limits?
According to US FDA
guidelines peak un-weighted sound pressure level should not be greater than 140
dB. Also, A-weighted root mean square sound pressure level should be greater
than 99dBA with hearing protection in place.
UK has provided
guidelines for operators as well, according to which hearing protection should
be provided to the operators who can be exposed at the average of 85 dB over 8
hour a day.
Exposure limits given
by Occupational Safety and Health Administration (OSHA)1
85dB(A) 16hrs a day
90dB 8 hrs a day
95db 4 hrs a day
100dB 2 hrs a day
105dB 1 hrs a day
110dB 0.5 hrs a day
115dB 0.25 hrs a day
What
are the noise reduction strategies?
1.
Modification in design of hardware
a) Use of active-passive shielded,
vibration isolated and vacuum enclosed gradient coils1
Gradient assembly can
be shielded so that eddy current is not induced in the surrounding metallic
structures in the MRI assembly. Active shielding refers to the use of secondary
coil other than primary gradient coil(X, Y, Z) that oppose and cancel out the
fringe field. Like primary coils there are three shielding coils. Passive
shielding refers to the use of conducting layers that are attached on the outer
radius of the gradient coil.
Gradient coil are
arranged such that structural or mechanical propagation of vibration into other
component is reduced this is called vibration isolated gradient coil. Also they
can be enclosed in vacuum to prevent air conduction of the vibration.
b)
Use of quiet gradient coil
Current
in the gradient coil are passed such that net Lorentz force is reduced.
2.
Passive noise control
Ear plugs and
headphones can be used to lessen the intensity by 10 to 30 dB. Disadvantage of
this method is that it interferes the verbal communication with patients.
3.
Active noise control8
It utilizes the sound, also
called anti phase sound that interferes destructively with the sound perceived
by the subject undergoing MRI. There are two main topologies for active noise
control. Feed forward and feed-back.
Feed-back
topology:
·
A microphone is placed near to the area
where attenuation is required.
·
It receives the sound generated by
scanner which is perceived by the subject and sends reference signal to the
loud speaker.
·
Loud speaker, on the basis of reference
signal sends control sound that interferes with the noise and produces
cancellation effect.
·
Disadvantage of this method is that
because of the time delay between production of control sound and reception of
the same by the subject, high frequency noise cannot be adequately suppressed,
making this sort of topology not suitable for EPI sequences where noise of
frequency 3 -4 kHz are generated.
Feed forward topology
· Microphone
is located near to the sound source which sends the reference signal in advance
to the loudspeaker.
· Another
microphone called “error” microphone is located near the subject and provides
electrical copy of residual noise.
· Advantage
of this topology is that higher frequency noise can be attenuated because the
reference signal is available on advance and can compensate for the delay due
to time required for the propagation of sound from loudspeaker to error
microphone. Thus this sort of topology can be used to reduce high frequency
noise from EPI sequences.
4.
Use of quiet pulse sequences9
Pulse sequence with
less gradient pulsing can be used. For example Gradient pulsing can be reduced
by using single shot sequences based on stimulated echo (STEAM).Further
reduction in gradient pulsing can be done by modifying the projection
reconstruction method in which the two gradient pulses are replaced by a single
mechanically rotating DC gradient coil.
Use of soft gradient
pulse is another option. Hennel et.al10 used band limited pulses
that used sinusoidal ramp with least number of slope (ramp) and maximum
duration of slope (ramp duration). Noise level was brought to as low as 30dBA
in GRE and SE and 60dBA in RARE sequence. Authors named such pulses as soft
pulse which can be obtained by convolving the hard pulses i.e the pulses with
rectangular waveform with the cosine window of length ᴦ (Figure 3)
Thus there is a growing
concern regarding the detrimental effects of acoustic noise generated in the MR
systems and the ongoing advancements in MRI hardware, especially in the gradient coil technology, are dedicated
towards development of a quiet scanner.
References
1.
MC.Jury
M,Shellock F.G Auditory noise associated with MR procedure:A Review J Magn Reson Imaging.2000 12:37-45
2.
Measuring
MRI noise
3.
Adriaan Moelker and
Peter M.T. Pattynama Acoustic Noise Concerns in Functional Magnetic Resonance
ImagingHuman Brain Mapping .2003;20:123–141
4.
Edelstein
WA, Hedeen RA, Mallozzi RP, El-Hamamsy SA, Ackermann RA, Havens TJ (2002):
Making MRI quieter. Magn Reson Imaging 20:155–163.
5.
Roozen
N.B ,Koevoets A.H and den Hamer A.J Active Vibration Control of Gradient Coils
to Reduce Acoustic Noise of MRI Systems.
6.
Hattori
Y,Fukatsu H,Ishikagi T :Measurement and evaluation of the acoustic noise of a 3 Tesla MR scanner Nagoya
J.Med.Sci,2009;69.23-28
8.
Chamber
J,Bullock D,Kahana Y.Developments in active noise control sound systems for
magnetic resonance imaging.Applied Acoustics 2007;68.281-295
9.
Alibek
S,Vogel M,Sun W etal.Acoustic noise reduction in MRI using silent scan:an
initial experience.Diagn Interv radiol 2014;20:360-363
10. F. Hennel,* F.
Girard, and T. Loenneker ‘‘Silent’’ MRI
With Soft Gradient Pulses Magnetic Resonance in Medicine ,1999;42:6–10