Dynamic MRI Scanning Technique of Pituitary Gland
In this technique, pre-contrast T1 Coronal and T1 Sagittal sequences of thin section 3mm through the sella are performed initially. Then, post contrast T1 Coronal and T1 sagittal are repeated. Post contrast T2 Coronal sequence is not a part of standard protocol but is useful for detecting cystic changes and hemorrhage.
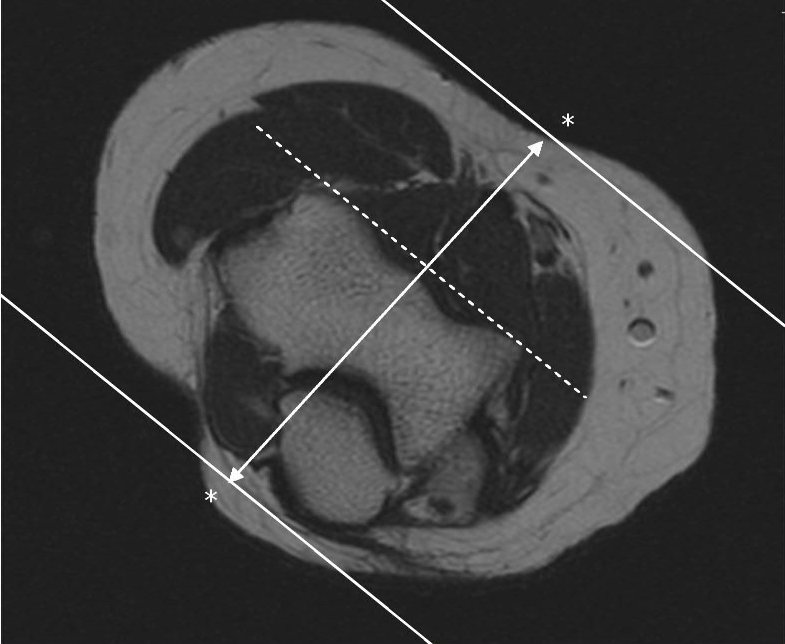
T1 Coronal thin is planned by making the mid scan line coincide the pituitary stalk. Cover the entire sellar and parasellar region.
T1 Sagittal thin is planned in mid T1 Coronal thin section image. The mid scan line runs through the pituitary stalk dividing the pituitary gland into equal halves.
This technique employs rapid sequential imaging to show temporal
difference in Gadolinium uptake between adenoma and normal gland. A series of MRI images are taken quickly over several minutes after Gadolinium has been injected. This type of scan is based on the idea that pituitary tumors and normal gland tissue absorb the dye at different speeds. In
this way, micro adenomas which enhance shortly after normal gland
enhancement can be identified. Macro adenomas can be easily detected on imaging. Micro adenomas are more difficult to detect because of smaller size, appear as a focal area of low signal on non-contrast T1 and also the peak enhancement of the microadenoma occurs after the normal tissue. Almost all pituitary tumors enhance, but
so does the normal pituitary gland. In fact, it enhances even more
brightly. However, compared to the normal pituitary gland (which
enhances quickly), most pituitary adenomas enhance more slowly because
of the disorganized microvasculature. We can take advantage of this
using a dynamic contrast study, even small pituitary tumors (as small as
1-2 mm) will show up when the MRI images are acquired while the
contrast is being injected because the normal pituitary gland will start
to enhance before the tumor, thereby showing the tumor more accurately
as a dark "shadow" within the brightly enhancing normal pituitary gland.
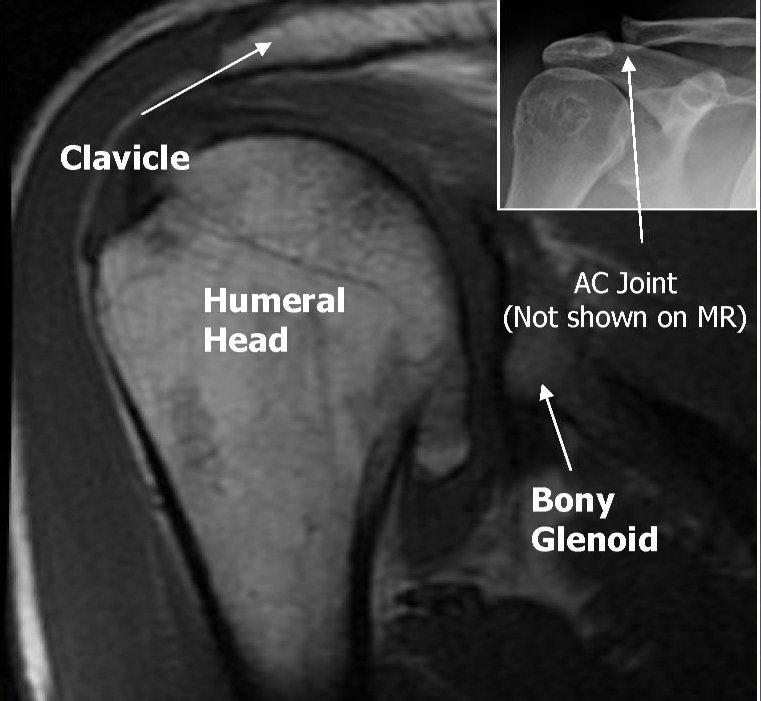
The T1 weighted image of the normal pituitary gland, stalk and cavernous sinus all increase in signal rapidly following administration of Gadolinium. A pituitary adenoma enhances less intensely than the adjacent normal tissue and appears as a focal hypointense area. A normal pituitary gland will usually look very white on a MRI after the dye has been used. The tumor will appear darker. On MRI, the normal anterior pituitary gland and its stalk return uniform isointensity relative to gray matter. These structures also show intense enhancement after the administration of contrast agent. The gland may be hyperintense in neonates and in pregnant women. The normal posterior pituitary appears bright on T1. The proteinaceous content of neurosecretory vesicles in posterior pituitary partly accounts for its appearance.
After the bolus injection of Gadolinium (Gadopentetate dimeglumine or Magnevist), 10 sets of images each consisting of three anatomic sections through the pituitary gland were acquired using T1 weighted Turbo Spin Echo sequence of 3 mm slice thickness with no intersection gap. This technique yields an imaging time 16 seconds per set and a total time of 2 minutes 40 seconds. Thenafter, brain survey using T2 Axial Turbo Spin Echo and T1 Axial Spin Echo post contrast can be done.
The enhancement fist occurs in the pituitary stalk, then in the pituitary tuft (the junction point of the stalk and the gland) and finally there is centrifugal opacification of the entire anterior lobe. Within 30-60 seconds, the entire gland shows homogeneous enhancement. The maximum image contrast between the normal pituitary tissue and microadenomas is attained about 30-60 seconds after the bolus. Most microadenomas appear as relatively non-enhancing (dark) lesions within an intensely enhancing pituitary gland. The peak enhancement of the pituitary adenomas occurs at 60-200 seconds, usually after the marked enhancement of the normal pituitary gland and persists for a longer duration. Delayed scan 30-60 minutes after contrast administration may demonstrate a reversal of the image contrast obtained at 30-60 seconds on dynamic scanning. This is because the contrast from the normal pituitary gland fades but diffuses into the microadenomas which stands out as a hyperintense focus. The addition of multiple sequences taken of the pituitary region gives an excellent picture of blood supply to the pituitary. So, the early enhancement of microadenoma long before anterior lobe attributes microadenomas having direct arterial blood supply similar to the posterior pituitary gland.
Reasearch had shown that the average time for on set of enhancement and peak enhancement of normal pituitary gland is 43 and 111 seconds respectively. Likewise, pituitary adenomatous nodules exhibited an average time 105 seconds for onset of enhancement and 188 seconds for peak enhancement. The average time for optimal tumor delineation is 93 seconds.
Please post your valuable comments!

 .
.